Make Your Site Healthier & Kinder
Are you the owner or manager of an online dating, hookup or sex app for gay men? If so, this part of the site is for you. We’ll give you some easy-to-follow ideas for how to integrate features into your site that make it a kinder, healthier, and more supportive environment for your users.
Maybe you’re interested in making it easier for your users to be able to access information about PrEP and STDs. Or you want to know how to help users self-identify as HIV-positive and undetectable. Or maybe you’d like to build in some features that help your users notify their partners if they test positive for an STD.
BHOC continues to provide data and ongoing consultations to owners to integrate sexual health features into their apps. Learn more: MSM who use dating app support new features to promote sexual health
Health Update Reminders
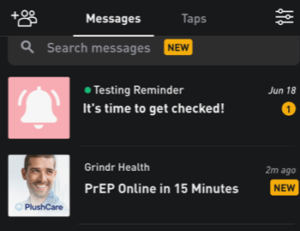
Dating sites and apps can play an important role in encouraging men to take care of their health. For example, Grindr has been promoting sexual health on its app by offering reminders to their HIV-negative and HIV-positive users.
Many of us change our sexual health practices over time. We may be using condoms during some periods, or PrEP during others; sometimes we know our viral load to be undetectable and sometimes we may not. For that reason, it’s good to encourage users to update their sexual health fields periodically to make sure they accurately reflect their own HIV status, test dates, and sexual practices. That will help users communicate more effectively with each other, and help them make informed choices.
Creating An Online Dating Profile
Go to Profile Options to learn how to structure profile options to allow users to disclose their HIV status and other relevant health information.
Resources for Trans Inclusivity
Cis men are not the only folks who use gay dating apps and sites to seek partners. Trans men and people with various gender identities also use these platforms to find partners. Many trans people face stigma online (and offline) from guys who have limited experience interacting with trans people, which not only leads to challenges in finding a partner, but can also make trans-identifying users feel unsafe. Making your site friendlier means making your site more inclusive to trans folks and making your site healthier means including educational resources about healthy sex that is specifically tailored towards the trans experience.
Below are resources that you can share with your users. The linked videos will help cis folk better understand what is like to be and date someone who is trans and the resource guides provide valuable sex ed information for trans people and their partners.
Resources
Resource Guides
- Safer Sex for Trans Bodies, Whitman-Walker Health & HRC Foundation
A safer sex guide for transgender and gender expansive people, and for their partners and lovers. Topics covered in the guide include: sex during and after transition, ways to talk to partner(s) (romantic, casual and transactional) about sex, suggestions for exploring your own sexuality, and STIs and condoms. For a copy in Spanish click here. - “Primed: A Sex Guide for Trans Men Into Men”, Gay Men’s Sexual Health Alliance
A sexual health resource written by and for gay, bi and queer trans men and their partners. Topics covered in the guide include: disclosure, finding sex and cruising, safer sex and harm reduction, HIV and other STIs, and more.
Video Resources
- Trans Men Discuss Online Dating, Boldly
- Trans Women Discuss Online Dating, Boldly
What’s partner notification?
Guys can get STDs all sorts of ways. Even if they’re taking very effective steps to prevent HIV transmission, such as PrEP or HIV meds, they can still get and transmit STDs.
In addition to condoms and testing, there’s another important step that men can take to help reduce STD and HIV transmission in their community: notifying their partners if they think they may have exposed them to an STD.
Many people with STDs never experience any symptoms, so unless they’ve been tested, they often don’t know they have an STD or that they could unknowingly give it to someone else. That’s why notifying partners that they may be infected is so vital to helping break the chain of transmission.
Research has shown that most men believe that notifying partners is the right thing to do, and many of them report wanting to do it themselves. But it can still be awkward, embarrassing, and sometimes even risky to tell a partner that they may have given them an STD. That’s why it’s important to give them easy ways to tell their partners.
Sites and apps can help. Here’s how:
1. Make it easier for men to keep track of their partners.
The more a site or app allows individuals to save messages or partner profiles, the easier it is for someone who’s been diagnosed with an STD to find a former partner. Allowing and encouraging users to save a profile or messages, can help a great deal. Adding capacity for users to save messages for a year would also be a tremendous help, since public health guidelines recommend that people infected with some STDs and HIV contact their partners met in the last year. Additional strategies, such as encouraging men to add people they’ve had sex with to their buddy or “favorite” list, would also help them keep track of their partners.
2. Allow Health Specialists on their sites and apps.
Health Specialists – sometimes called Disease Intervention Specialists, or DIS, – are highly trained in and for decades have played an essential role in stopping the spread of STDs and HIV by helping people get tested and treated. They’re employed by either a health department or a community-based organization. DIS are also using their skills in contact tracing for COVID-19.
Healthcare providers are required by law to report certain STDs to their local health department. Once someone is diagnosed with syphilis or HIV by a healthcare provider, a health specialist will get in touch with them. (Some health departments will also have a health specialist contact a patient with gonorrhea if they have enough staff to do so.) They’ll offer to work with the patient to tell their sex partners that they may have been exposed and encourage them to go to their doctor or a clinic to be tested. Working with health specialists is always completely voluntary.
If a site user is uncomfortable telling their partners directly, they can ask a health specialist to help by reaching out to partners to let them know that they have been exposed to an STD or HIV. The health specialist will NEVER tell a partner who gave them their name. Health specialists are committed to protecting privacy. Furthermore, health specialists will not give any details that would reveal where, or when, the partner may have been exposed.
Creating a standardized profile for a health specialist, with their agency’s logo, is one key step to promoting partner services on a site or app.
Importantly, research has found that site users report welcoming the help of a DIS to notify their partners.
Again, most men want to let their partners know about a potential STD and are glad that their partners are notified and able to get tested and treated. And many men who get notified are grateful that they got the information so that they can take care of themselves. Ultimately, by people notifying each other, either by themselves or with the assistance of their health department, they’re promoting the health of the entire community.
Partner notification has lent itself much more to websites than apps. First, site users have unique identities, which make it easier for a user to find a partner. Second, unless a user has saved a partner’s profile, he may not be able to see him if he’s not in the same geographic area. This also makes it much harder for them to notify partners, as well as for health specialists to find them if they’re trying to help.
BHOC is currently working with researchers at the University of Washington to determine which strategies app users would be most likely to support, including allowing users to anonymously notify partners within an app that they should get tested, and will continue to work with app owners to find ways that work for them.
Tellyourpartner.org - Anonymous Text and Email Partner Notification Platform
Tellyourpartner.org is a brand-new platform for individuals recently diagnosed with an STD who want to notify their partners anonymously by text or email. Users may choose a pre-populated message or write one of their own, and notify up to six partners at a time.
Internet Partner Services: History & Effectiveness
The first documented instance of the Internet being used for the purposes of notifying partners that they may have been exposed to an STD and should get tested was in 1999, and was a response to a syphilis outbreak in San Francisco attributed to sexual encounters that were facilitated through a chat room.23 In the same year, another study was conducted that focused on the Internet as a sex-seeking environment and was identified as a possible STD/HIV risk environment.9
As a result of a significant increase in the number of STD patients reporting sex partners met online through chat rooms, social networking, and hook-up sites, public health programs began incorporating the internet and email into their partner services programs.24-26 These early efforts showed that Internet-based partner services (IPS) held promise as a legitimate tool when partnered with other traditional methods for disease prevention.
The CDC supports using dating websites as a strategy to find partners. By September of 2005, CDC had responded to the promising outcomes shown in several areas with a “Dear Colleague Letter” to public health departments 4 that encouraged program areas to explore the Internet as a disease intervention and prevention tool. A second CDC “Dear Colleague Letter” supporting the use of the internet for partner services was released in 2010.5
Since the release of the first Dear Colleague letter, several studies have been conducted to evaluate IPS outcomes by assessing rates of partner elicitation, notification, and testing and quantifying the number of partners who otherwise would not have been contacted without IPS.
In Texas, Vest et al found that the use of email to reach partners for whom no other contact information was available resulted in 50% of those partners being notified, of which 26% were found to be infected with an STD. Additionally, they found that sending emails did not require additional staff time, and allowed for rapid partner notification (PN) communication.27
Ehlman et al. assessed the effectiveness of Internet partner services in Washington, D.C. and found Internet partner notification (IPN) improved notification and treatment for early syphilis. Using IPN led to a 75% increase in the number of partners investigated, and a 26% increase in number of partners examined and treated, when necessary. At least 285 partners who would not have otherwise been contacted were notified of exposure.28
In addition to emails, social networking sites can also be a venue for PN. The Milwaukee Health Department in Wisconsin reported on the use of the social networking site, Facebook, to augment partner notification efforts involving a syphilis cluster (n=55). Within the cluster, 17 positive cases of syphilis were found, 10 of which were co-infected with HIV. Among the cluster, two of the positive cases had been named as Facebook contacts, and as a result, were able to be located by Disease Investigation Specialists, or DIS (also known as Health Specialists), when traditional methods failed. Moreover, these two cases were found to be key connectors within the cluster. Facebook was also used to augment traditional partner notification for an additional five individuals. Hunter et al (2014) found that the use of Facebook augmented traditional efforts by allowing DIS to reach partners more quickly, especially among those individuals who may frequently change phone numbers or addresses.29
More recently, texting has also been shown to be a very effective way of reaching partners. In a 2011 Letter to the Editor, Kachur et al. described a case in which text messaging was successfully used for partner notification. In this case, DIS in the New York State Department of Health were able to reach and notify a partner of their syphilis exposure through text messages after traditional efforts had failed.15
In 2012, Mendez et al reported on Multnomah County’s texting PS program, which consisted of sending a text message for partner notification immediately following an attempt to reach cases by phone, but before mailing letters or conducting a field visit. Text messages were sent to 149 clients immediately following an attempted to reach them by phone; 56% of those texted responded to DIS with a phone call, many within 10 to 15 minutes. They also found texting reduced the need for mailing letters and making field visits.30
Hightow-Weidman et al evaluated the use of text messaging for the partner notification of 29 contacts in North Carolina. Text messaging was used only after traditional or IPN attempts did not elicit a response. Of the 29 contacts, 48% (n=14) responded to the text, all within in a median time of 57.5 minutes. Among the 14, two new cases of syphilis and one new case of HIV were identified.31
Udeagu et al. compared traditional, internet and text-based (txtPS) PS delivery methods on contact, notification, and HIV testing rates. They found the contact rates for txtPS (77%) to be significantly higher than traditional PS (69%) or IPS (41%; p<0.0001). IPS (odds ratio (OR), 2.1; 1.2-3.4) and txtPS (OR, 2.4, 1.7-3.2) resulted in a greater likelihood of notifying partners than traditional PS (p<0.0001), but traditional PS yielded the highest proportion of partners testing for HIV (69% versus 34% and 45%, respectively; p<0.0001). They concluded that augmenting their PS program by incorporating the three modes of PS improved their overall PS outcomes, reached partners who were otherwise unreachable, and improved their operational efficiency.32
Lastly, Pennise et al reported on the Monroe County Department of Public Health in New York, which has, since 2012, issued smart phones to the DIS for use during field investigations. They reported on a cluster investigation conducted between February and May 2013 through which partner elicitation, notification, and testing was improved through the use of smart phones. Use of smart phones allowed DIS to search online sites and mobile applications with patients in order to elicit partner information in real time. These efforts resulted in seven new cases of disease being diagnosed, including two new cases of HIV.22
In addition to augmenting traditional partner services, partner notification through an online community is considered an acceptable tool by members of that community. In a national IPS study performed by The Fenway Institute, Fenway Community Health looked at the acceptability of IPS among men who have sex with men (MSM). A total of 1,848 MSM were recruited online via an Internet sex partner-seeking website between October and November 2005. The study concluded that IPS should be considered an acceptable tool for partner services, with more than 92% of participants reporting that they would use IPS in some capacity to inform their sexual partners of possible exposure, if they were to become infected with an STD in the future.33
Additionally, BHOC assessed the levels of support for partner notification by users, website owners, and public health in 2009. Two-thirds of the website users welcomed internet partner services by the government. Currently, BHOC is also working with University of Washington researchers to assess interest in mobile-app based partner notification strategies. Initial analysis suggests that while users believe they themselves should notify their partners, they still welcomed assistance by public health agencies. Since its inception in 1999, IPS has become a standard practice in many health departments. IPS has been an effective tool for the elicitation, notification, and testing of partners and for reaching those partners, who otherwise would not have been notified of their exposure to an STD or HIV.
Adapted from CDC
The Future
Partner notification has lent itself much more to websites than apps. First, site users have unique identities, which make it easier for a user to find a partner. Second, unless a user has saved a partner’s profile, he may not be able to see him if he’s not in the same geographic area. This also makes it much harder for them to notify partners, as well as for health specialists to find them if they’re trying to help.
